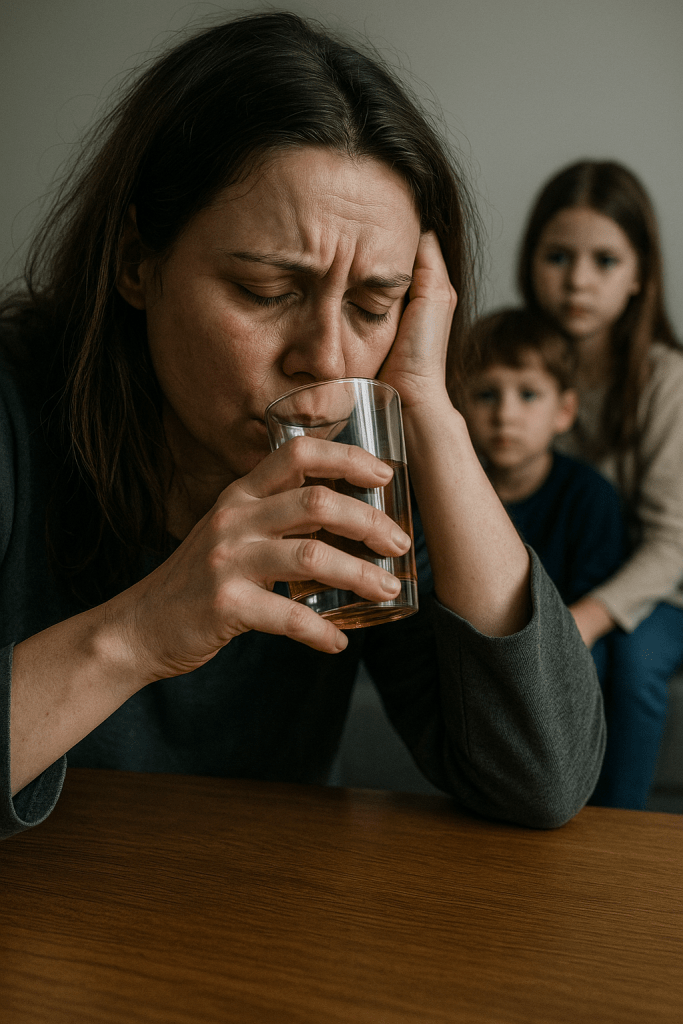
Alcoholism — or alcohol use disorder (AUD) — is more than “drinking too much.” It’s a chronic condition that changes the brain, hijacks decision-making, and affects health, relationships, and self-worth.
Because alcohol is legal and socially accepted, the line between “casual drinker” and “problem drinker” can be blurry — until it’s not.
This guide is designed to be your pocket tool: clear, practical, and easy to use whether you’re learning for yourself, for someone you love, or for professional interest.
When Can It Start?
Alcoholism can develop at any age — from late teens experimenting at parties to midlife professionals who start using it to “unwind” after work.
Often, it begins with drinking for stress relief, sleep, or social comfort. Over time, tolerance builds, meaning you need more for the same effect. That’s when the slide can begin.
Is It in the Genes?
Research suggests 40–60% of the risk may come from genetics. If alcoholism runs in your family, your risk is higher — but genes are not destiny.
Environment, coping skills, mental health, and even cultural attitudes toward alcohol can tip the scale either way.
Warning Signs
- You drink more or longer than planned.
- You’ve tried to cut down but couldn’t.
- Drinking interferes with work, studies, or relationships.
- You feel anxious or shaky without alcohol.
- You drink in dangerous situations (before driving, with certain medications).
Is It Curable?
There’s no instant “cure,” but alcoholism is treatable and recovery is possible. Think of it like diabetes: it can be managed, and you can live a healthy, fulfilling life with the right tools.
How Alcoholism Can Be Treated — Methods That Work
Different approaches help in different ways, and often a combination gives the best results.
1. Medical Detox
How it helps:
For heavy drinkers, suddenly stopping can cause dangerous withdrawal (seizures, delirium tremens). Medical detox in a clinic or hospital provides 24/7 monitoring, fluids, and medication to make withdrawal safer and more comfortable.
Best for: People with severe dependence or previous dangerous withdrawals.
2. Rehabilitation Programs
How it helps:
- Inpatient rehab (living at a facility) offers a structured, trigger-free environment.
- Outpatient rehab allows people to stay at home while attending daily or weekly therapy.
Both combine counseling, education, and skills-building.
Best for: Those who need intensive support, especially in early recovery.
3. Therapy & Counseling
How it helps:
- CBT (Cognitive Behavioral Therapy): Identifies and changes thought patterns that lead to drinking.
- Motivational Interviewing: Helps build personal motivation for change without pressure.
- Trauma therapy: Addresses unresolved issues that may fuel drinking.
Best for: Anyone wanting to understand why they drink and how to replace it with healthier coping skills.
4. Support Groups
How it helps:
- AA (Alcoholics Anonymous): A 12-step program focusing on peer support and spiritual growth.
- SMART Recovery: Evidence-based tools for self-management, no spiritual component.
They offer understanding from people who’ve been there, and accountability to keep going.
Best for: Those who benefit from community support.
5. Medication-Assisted Treatment
How it helps:
- Naltrexone: Blocks alcohol’s pleasurable effects, reducing the urge.
- Acamprosate: Helps normalize brain chemistry after quitting.
- Disulfiram: Causes unpleasant reactions if you drink (deterrent).
Best for: People who relapse frequently or have strong cravings.
6. Holistic & Alternative Approaches
How they help:
- Mindfulness & meditation: Reduces stress and helps you ride out cravings.
- Yoga & breathwork: Supports emotional regulation and physical recovery.
- Acupuncture & herbal remedies: Used in some cultures to ease cravings (effect varies).
- Ayahuasca-assisted therapy: Explored in South America for deep emotional healing — controversial and should only be done in legal, supervised settings.
Best for: Those who want a mind-body-spirit approach alongside medical or psychological treatment.
7. Contingency Management (CM)
What it is:
A behavioral therapy that uses small rewards for achieving sobriety milestones (negative alcohol tests, attending therapy).
How it works:
Rewards reinforce positive behavior until sobriety habits strengthen internally.
Best for: People who respond well to structure and tangible motivation.
Evidence: Strong results in reducing substance use, especially when combined with counseling.
8. Community Reinforcement Approach (CRA)
What it is:
Therapy that focuses on replacing the lifestyle connected to drinking with new, rewarding activities.
How it works:
Teaches coping skills, builds sober social networks, improves family relationships, and addresses work or housing issues.
Evidence: Proven effective for both alcohol and drug addiction, especially long-term.
9. Dialectical Behavior Therapy (DBT)
What it is:
Originally for borderline personality disorder, now used for addictions.
How it works:
Teaches mindfulness, emotional regulation, and distress tolerance to manage urges.
Best for: People with intense emotions, trauma, or co-occurring mental health issues.
What it is:
Using genetic testing to match patients with the most effective medication (e.g., certain genetic profiles respond better to naltrexone).
Evidence: Still emerging, but promising for personalized addiction medicine.
11. Neurofeedback
What it is:
Brain training using EEG to help regulate brain activity.
How it works:
Teaches the brain to shift from craving/stress states to calmer, more focused states.
Evidence: Mixed, but some studies show reduced cravings and improved emotional stability.
The Role of Psychology
Psychology is the bridge between quitting drinking and staying sober. It helps:
- Identify triggers (stress, social pressure, loneliness).
- Build new coping strategies.
- Heal the guilt, shame, and broken trust alcoholism often leaves behind.
How to Support Someone in Recovery
Friends can:
- Listen without judging.
- Offer healthy distractions (walks, hobbies, outings without alcohol).
- Encourage help-seeking without pushing.
Family can:
- Educate themselves about alcoholism.
- Set boundaries (no alcohol in the house, no covering up mistakes).
- Join family support groups like Al-Anon.
What to Say / Never Say
Say:
- “I care about you and I’m here.”
- “I’m proud of your effort.”
- “You’re not alone in this.”
Never Say:
- “Just stop drinking.”
- “If you loved me, you’d quit.”
- “You’re hopeless.”
Handling Relapse
Relapse is common — it’s not the end, it’s part of the process for many. The key is to act quickly:
- Identify what triggered it.
- Get back into meetings, therapy, or medical care.
- Remind them they haven’t “lost all progress” — every sober day counts.
Typical Sentences People with AUD May Say
- “I can stop whenever I want.”
- “It’s just one drink.”
- “Everyone drinks this much.”
- “I’m under a lot of stress.”
Useful Resources
- NIAAA – National Institute on Alcohol Abuse and Alcoholism
- Alcoholics Anonymous
- SMART Recovery
- WHO – Alcohol Fact Sheet
Final thought: Alcoholism is complex — a mix of biology, psychology, and environment. No one is immune, and no one is beyond help. With the right combination of methods, support, and personal commitment, recovery is not just possible — it’s happening every day.
